Why Women's Heart Health?
While heart disease is on the decline among men, it is rising among women.
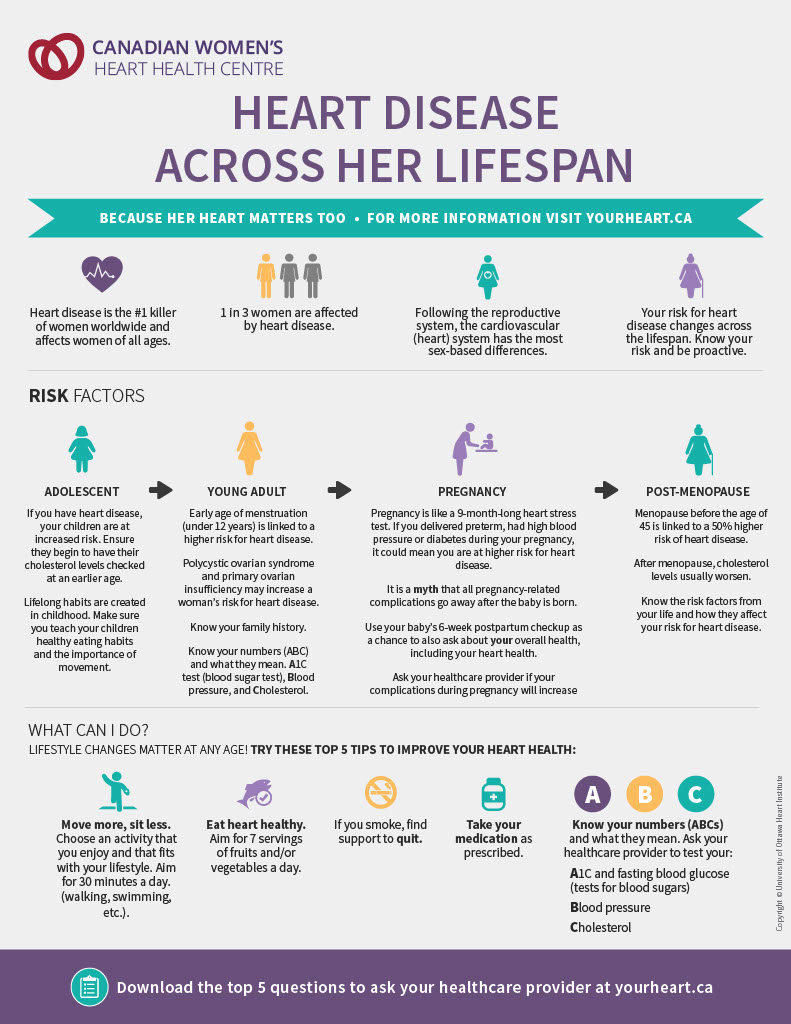
Heart disease is the number one killer of women worldwide and the leading cause of premature death in women in Canada.
Much of what we know about the diagnosis and treatment of heart disease – including conditions of the heart, its valves, arteries and other blood vessels – is based on research in men, but women’s hearts and the way they experience heart disease are different in many ways.
These differences are important because they can affect how heart disease presents in women, and how it’s diagnosed and treated. It also affects women’s survival rates.
With the right information and action, it’s possible to prevent heart disease or improve your chances of surviving it to lead a healthy life. The Canadian Women’s Heart Health Centre can help you take the first easy steps toward a healthier heart by arming you with information.
Women’s hearts are different.
Women generally have higher heart rates and smaller hearts and arteries than men. They have less buildup of plaque in their arteries, and the plaque they do have tends to behave differently.
While male hormones enlarge arteries, female hormones make them smaller, making women’s arteries more prone to blood clots or blockages and more difficult to repair.
Some risk factors are different.
The traditional measures of risk underestimate the dangers for women. While men and women share the most of the same traditional risk factors, some risk factors carry a stronger relative risk in women. Smoking, diabetes, high blood pressure and a family history of heart disease are red flags for women in particular.
The following conditions can lead to a greater risk of heart disease for women:
Certain pregnancy complications
Ex. premature birth, diabetes or hypertension during pregnancy, preeclampsia
Earlier than average menopause
Polycystic ovary syndrome (cysts in ovaries and hormonal imbalance)
Systemic inflammatory and autoimmune disorders
Ex. rheumatoid arthritis, lupus
Cigarette smoking
Women have a 3x higher risk of heart attack due to cigarette smoking compared to men.
Diabetes
Women living with diabetes are 3x more likely to die from heart disease compared to men.
Women’s symptoms can be different.
Women’s symptoms often differ from the classic symptoms seen in men. While both men and women often report angina – sharp and crushing chest pain – leading up to a heart attack, many women also experience an ache across the upper back and in the stomach, as well as shortness of breath and extreme fatigue.
Because symptoms in women can be less specific, they can be harder to recognize as danger signs.
Heart attack symptoms most often felt by women:
- Chest pain, pressure, tightness, or burning
- Pain in the jaw, neck, right arm, or back
- Extreme sweating
- Shortness of breath
- Stomach pain, nausea or indigestion
Other symptoms women may feel:
- Profound fatigue
- Sleep problems
- Dizziness or light-headedness
- Fast or irregular heartbeat
Did you know?
Women are more likely to present with 3 or more symptoms in addition to chest pain.
If you think you are having a heart attack, get help right away. If possible, call 911. Do not drive yourself.
Women develop heart disease later in life.
Most women experience their first symptoms or heart attack after the age of 65, while for men the onset is often earlier. But the build-up of artery-clogging plaque can begin as early as the age of 20, so it’s important to take care of yourself at every age.
It’s believed that estrogen protects most younger women from heart complications but once estrogen levels drop during menopause, the risk of heart disease rises.
Being older also means women are more likely to have other conditions, such as diabetes, that further complicate the identification and treatment of heart disease.
Heart disease often looks different in women.
Most guidelines for diagnosing heart disease have been based on studies of male patients. For example, current medical guidelines for diagnosing coronary artery disease focus on detecting a kind of damage to the arteries that is more common in men than in women. The result can be missed or delayed diagnosis for women, leading to delays in treatment.
In the last 15 years, new research on heart disease in women has produced valuable evidence to help inform new medical guidelines.
Women and men can have different types of heart disease.
Common types of heart disease:
- Cholesterol build-up in heart blood vessels (coronary artery disease)
- Leaky or stiff heart valves affecting blood flow (valvular heart disease)
- Irregular or rapid heartbeat (arrhythmia)
Women are more likely to have:
- Tear in large blood vessels of the heart (spontaneous coronary artery dissection, SCAD)
- Tightening of the large blood vessels of the heart, limiting blood flow (coronary vasospasm)
- Small vessel disease (microvascular dysfunction)
- Weakened heart due to a stressful event (Takotsubo cardiomyopathy)
- Weakened heart during or after pregnancy (peripartum cardiomyopathy)
Women test differently.
Some diagnostic tests long considered standard in cardiology have given inconsistent or confusing results for some categories of women.
Despite new research regarding testing for heart disease in women, there is still debate over which tests and diagnostic strategies are the most effective.
Women may get treated differently.
Women are under-studied and under-diagnosed when it comes to heart disease, leading, in many cases, to under-treatment. Many people, and some medical practitioners, are still unaware that women have a higher rate of death from heart disease than men, that their symptoms are often different, and that they may require a different diagnostic approach.
The result is that women don’t always get the most appropriate treatment because the severity of their illness is underestimated.