Chest Pain in the Emergency Department
Women are 7 times more likely to be sent home from the Emergency Department.5
The Assessment of Women Presenting to the Emergency Department with Chest Pain
Chest Pain in Women in the Emergency Department: A Focus on Acute Coronary Syndrome
A point-of-care emergency clinical summary has been created for Acute Coronary Syndromes (ACS) in women. This core document will be accompanied by additional documents/tools focusing on specific conditions that can cause Myocardial infarction with non-obstructive coronary arteries (MINOCA).
The BC Emergency Medicine Network was the first dissemination point, with further dissemination on the horizon. The development of these women’s heart health-specific tools, including checklists and flowcharts, will support front-line decision-making.
Scope of the Problem
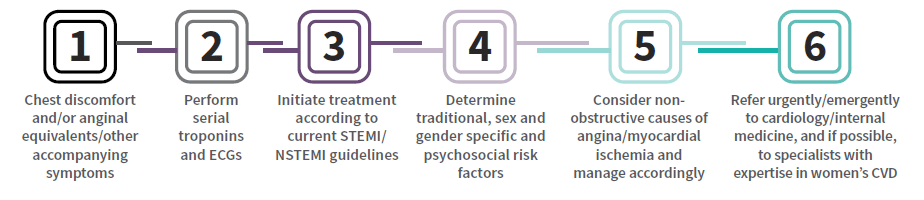
Cardiovascular disease (CVD) is the leading cause of premature death in women in Canada1. Mortality rates in men have stabilized in the last decade but have continued to increase in women in Canada2 and can occur for women of all ages. Sex and gender-specific differences exist in awareness, symptom presentation, diagnosis, prognosis, and treatment3. The diagnosis of acute coronary syndrome (ACS) in women presenting to the ER can be complex and challenging. Rapid diagnosis and treatment are vital.
Symptoms
More than 50% of women who experience heart attacks have their symptoms unrecognized by healthcare providers4. In addition, women are 7x more likely to be sent home5. Chest discomfort is the most common presenting complaint in 90% of ACS, in BOTH men and women4.
Women may, however, describe their symptoms differently than men, as discomfort or pressure rather than “pain.” Anginal equivalents, such as dyspnea, epigastric pain, and upper back discomfort, are more often reported in women, and may lead to misdiagnosis and delays in treatment. Heart attacks are on the rise and can occur in women of all ages. Assessing for cardiac disease should be prioritized in women who experience chest pain/pressure.

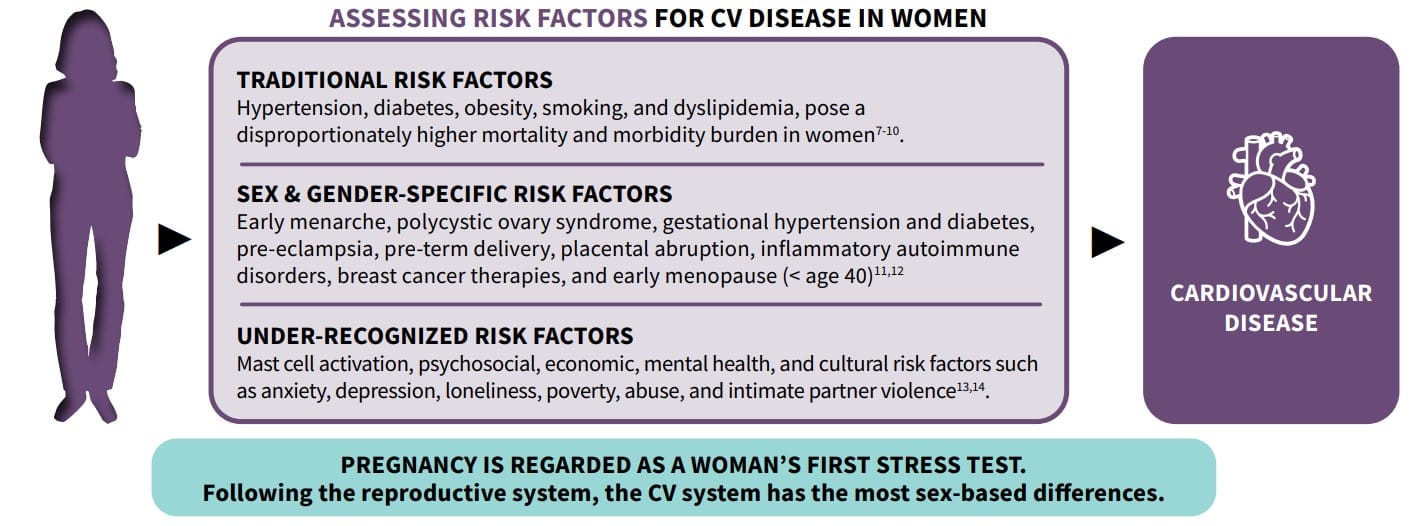
Risk Factors
Cardiovascular risk assessment in women requires evaluation of traditional, sex-gender specific, and under-recognized risk factors6:
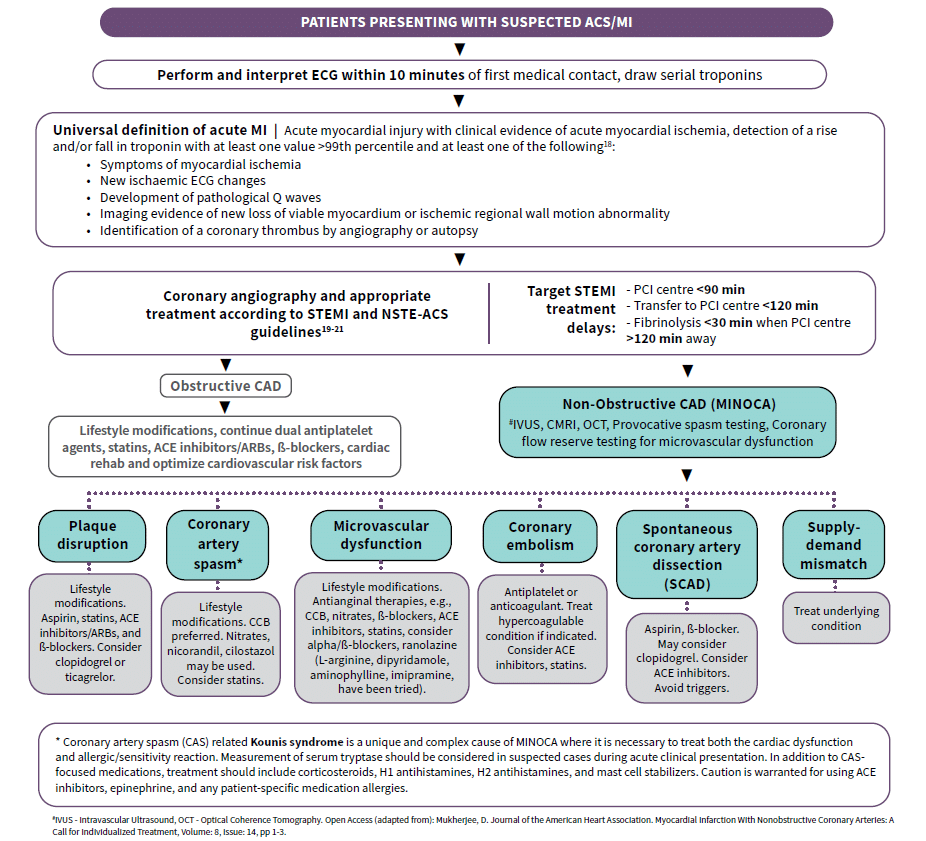
Pathophysiology
CAD, is a type of CVD that can be obstructive or non-obstructive. Obstructive coronary artery disease (ST and non-ST elevation myocardial infarction) is common in both men and women. However, in 5-15% of ACS cases, MINOCA can occur, particularly in women15. The coronary angiogram in MINOCA reveals < 50% stenosis in any major epicardial artery. Serial troponins, preferably high-sensitivity assays, using sex-specific thresholds, are critical, as initial results may be normal. Initial troponin should be followed by repeat sample collection 1-3 hours later for high-sensitiviy troponin and 3-6 hours later for conventional troponin assays16. Long term prognosis for MINOCA patients may include worse quality of life indicators, compared to obstructive MI patients.
Potential Causes of MINOCA
Possible causes of MINOCA include, but are not limited to, plaque rupture/erosion, coronary artery vasospasm (including ACS syndrome accompanying mast cell activation from allergic, hypersensitivity, or anaphylactic reactions: Kounis syndrome)17, microvascular dysfunction, coronary artery embolism, and spontaneous coronary artery dissection (SCAD)15.
Investigations and Medical Therapy
Differential Diagnosis
ACS in Women Checklist
Acknowledgements
This educational material is brought to you by the Knowledge Translation and Mobilization Working Group (KTMWG) of the Canadian Women’s Heart Health Alliance (CWHHA). The composition team includes Dr. Shahin Jaffer, Dr. Christine Pacheco, Dr. Najah Adreak, Dr. Jill Bruneau, Helen Robert, Karen E. Jacques, and Meagan Noble. The CWHHA is powered by the Canadian Women’s Heart Health Centre at the University of Ottawa Heart Institute.
